Keratoconus
Keratoconus
What is Keratoconus?
Keratoconus, often referred to as “KC,” is a non-inflammatory eye condition in which the typically round dome-shaped cornea progressively thins and weakens, causing the development of a cone-like bulge and optical irregularity of the cornea. This causes “static” in your vision and can result in significant visual impairment.
Keratoconus Signs and Symptoms
Keratoconus typically first appears in individuals who are in their late teens or early twenties and may progress for 10-20 years and then slow or stabilize. Each eye may be affected differently. In the early stages of keratoconus, people might experience:
The cornea is responsible for focusing most of the light that comes into the eye. Therefore, abnormalities of the cornea, such as keratoconus, can have a major impact on how an individual sees the world, making simple tasks such as driving a car or reading a book very difficult.
Corneal Cross-linking
What Is iLink™ Corneal Cross-Linking?
iLink™ corneal cross-linking is a minimally invasive outpatient procedure that combines the use of ultraviolet light and specially formulated eye drops to stiffen and strengthen corneas that have been weakened by disease or refractive surgery. Cross-linking is considered the standard of care around the world for progressive keratoconus and corneal ectasia following refractive surgery.
At Eye Specialists & Surgeons of Northern Virginia, we perform the FDA approved, “Epi-Off” technique. This entails the use of a surgical instrument to gently brush off the surface cells of your cornea, known as the epithelium. By removing the top layer of cells, the riboflavin eye drop penetrates deeper into the cornea allowing for better results. The epithelium that is removed regenerates back on its own. This may take a few days to occur so the patient should plan on some initial downtime to recover.
Is iLink™ Corneal Cross-Linking Covered by Insurance?
The medical necessity of iLink™ has become widely recognized. As a result, commercial insurance coverage for the procedure is now over 95% in the United States.
Benefits of Corneal Cross-Linking
Riboflavin
Under the conditions used for iLink™ corneal cross-linking, specially formulated pharmaceutical-strength riboflavin eye drops called Photrexa® (riboflavin 5’-phosphate ophthalmic solution) and Photrexa® Viscous (riboflavin 5’-phosphate in 20% dextran ophthalmic solution) help enable the cross-linking reaction.
Ultraviolet Light (UV)
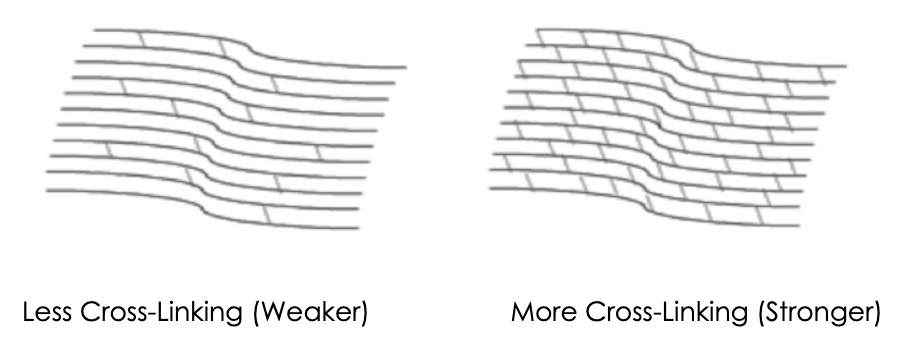
iLink™ corneal cross-linking applies an artificial source of ultraviolet light from a machine called the KXL System once the cornea has been soaked in the Photrexa® and Photrexa® Viscous eye drops. This process works to stiffen the cornea by increasing the number of molecular bonds, or cross-links, in the collagen.
Combining Riboflavin and UV Light
Using Photrexa® and Photrexa® Viscous riboflavin eye drops, combined with ultraviolet light from the KXL system, the iLink™ procedure stiffens and strengthens the cornea to slow or halt progressive keratoconus.
Corneal Cross-Linking Procedure – What to Expect
Corneal Cross-Linking is an eye treatment that may be done in office. There are 3 steps. 1) Your ophthalmologist will numb your eye with drops and then gently remove part of the outer layer of your cornea. 2) The ophthalmologist will put special vitamin eye drops (riboflavin) in your eye many times over 30 minutes or more. 3) The ophthalmologist will shine a special ultra-violet (UV) light on your eye for another 30 minutes and keep adding drops. The vitamin eye drops and UV light work together to make the collagen stronger. The cornea becomes stiffer and usually stops bulging out.
Common Symptoms during Recovery:
- It is common to experience varying degrees of discomfort beginning 30 to 90 minutes following the surgery as the numbing drops begin to wear off. Many patients describe this sensation as feeling like an eyelash is in the eye or lodged beneath the contact lens. This rarely lasts more than a few days and is a normal part of the healing process. Remember that the doctor will put a contact lens in your eye directly after surgery to act as a bandage. It is important not to remove the contact lens for any reason because without it, the pain will increase and your eye may not heal normally.
- A contact lens that has fallen out accidentally should NOT be reinserted. If you do so, the contact lens has likely been contaminated therefore increasing the risk of infection, which could permanently affect your vision. Instead, continue using your eye drops, gently tape the eye closed and call us at (571) 349-2191 so that we can insert a new contact lens that same day or the following morning.
- The bandage contact lens in combination with lubricating drops, prescription eye drops (to be used as directed by the surgical team) and mild, oral analgesics should provide relief. Also, you can place a cold washcloth or an ice pack over the eye to help relieve discomfort (10 minutes on, 10 minutes off and repeat as needed). In most cases, the bandage contact lens will be removed by the doctors on the 4th or 5th postoperative day. After this, the eye will become more comfortable, and your vision will begin to improve.
- You may experience watery eyes, a runny nose, light sensitivity and eye redness during the early postoperative period. This is normal and is caused by the post-surgical eye irritation.
- You may experience “hazy” vision during the recovery period. The vision should begin to stabilize after the bandage contact lens is removed from your eye. Although visual recovery is slower for some patients, most experience improved vision within the first several months. Vision one month after surgery is often somewhat hazed due to normal healing with collagen cross-linking. Corneal topography usually shows an artificial worsening of corneal shape one month after surgery with progressive improvement thereafter for over a year in most cases.
- Some patients have dry eye symptoms causing a sandy sensation or eye tenderness. This may persist for several months following the surgery and is best treated with frequent artificial tear use.*** To promote healing and to help hazy vision during the recovery period, your Ophthalmologist may insert an amniotic membrane (Prokera).
- Infection is very rare but is the most serious problem that can present after this procedure. It is important to be evaluated immediately if you experience extreme pain, eye redness, sudden blurred vision and/or discharge.
- It is very important that you make it to all of your postoperative examinations so that if any changes or complications arise, they can be addressed immediately.
- You may resume contact lens wear when cleared by the doctor. This is typically three to four weeks after the procedure. Once you resume contact lens wear, it is asked that you discontinue contact lens wear three days before subsequent postoperative appointments to ensure the contact lens is not warping the cornea before measurements are taken. It is important to have a consistent protocol for discontinuing contact lenses before these appointments. If this is difficult for you to coordinate, please discuss with your provider to make a plan.
Day of Corneal Crosslinking:
Is Cross-Linking Right for Me?
Patients who have been diagnosed with progressive keratoconus or corneal ectasia following refractive surgery should ask their doctor about iLink™ corneal cross-linking.
We at Eye Specialists and Surgeons of Northern Virginia are proud to offer patients the first and only FDA-approved therapeutic solution for the treatment of progressive keratoconus. Now, patients who once had little to no therapeutic option to treat keratoconus have the opportunity to slow or halt the progression of this sight-threatening disease.
CTAK -Keratoplasty for Addition Tissue Corneal
CTAK is the latest advancement in keratoconus treatment, focused on accuracy and precision for both patients and surgeons. This innovative procedure involves the use of a CTAK inlay, designed to optimize corneal flattening, improve visual acuity, and add thickness to the cornea.
Using a Ziemer Neo Z8 Femtosecond Laser, CorneaGen processes tissue to the precise parameters for each patient. The tissue is sterilized, packaged and shipped with a custom surgical plan.
Advantages
CTAK creates an offering to improve outcomes by treating each patient for the unique progression of keratoconus they’ve experienced.
Recommended Patients
Moderate keratoconus: 50D-80D. Patients with ectasia need more care and can schedule a consultation.
First CTAK Case
ICL-CTAK
What is the difference between CAIRS (Corneal Allogenic Intrastromal Ring Segments) and CTAK?
These terms are often used interchangeably. CTAK utilizes a specific proprietary nomogram to determine the exact size of the segments needed for optimizing corneal treatments. A femtosecond laser is then employed to create the precise channel. Over time, however, CAIRS has evolved internationally, and many treatments are now also performed using a femtosecond laser along with a developed nomogram. Ultimately, both methods aim for the same goals and are moving toward similar outcomes and procedures.
The Doctors at Eye Specialists & Surgeons of Northern Virginia have either authored or reviewed and approved this content.


