What Is A Cataract?
What Is A Cataract?
Overview
Cataract is a clouding of the natural lens, which is situated inside the front portion of our eyes. Through time, this lens thickens and loses transparency due to protein misfolding caused by the natural aging process as well as other environmental factors.
Symptoms
Cataract formation can cause different types of visual disturbances. Symptoms include but are not limited to:
- Cloudy or dim vision
- Difficulty with nighttime driving
- Increased halos around lights
- Frequent changes in glasses or contact lens prescriptions
- Requiring brighter light to read or do other activities
If you are experiencing one or more of these symptoms, it might be time to consider a cataract evaluation. Although cataracts are not harmful to our eyes, waiting too long can result in a difficult surgery. Therefore, a yearly dilated exam is recommended to track progression and ensure eye health.
There are about 26 different types of cataracts and they can be classified based on cause, location on the lens as well as the speed of progression.
Nuclear Sclerotic Cataract
Also known as, Age-Related Nuclear Sclerosis, this type of cataract is usually associated with aging. It is typically slow progressing and presents as a gradual yellowing and hardening of the central portion of the lens.
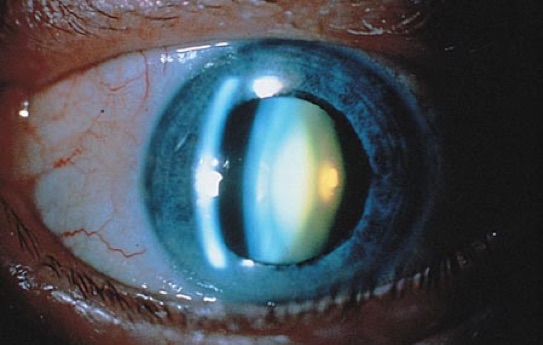
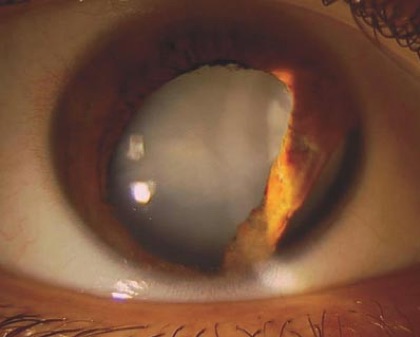
Cortical Cataract
Occurring in the lens cortex, white opacities begin in the periphery of the lens and work their way towards the center. Individuals with this type of cataract strug-gle with glare and are debilitated by nighttime driving.

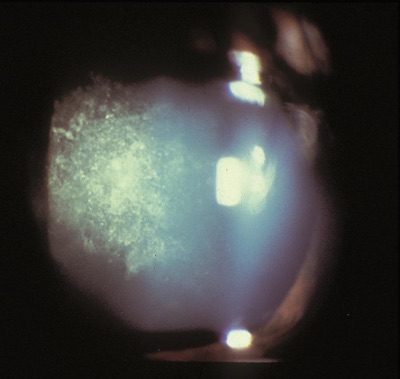
Posterior subcapsular cataract
These types are often seen in younger patients. They pre-sent as a sheen-like opacity and occur in the back of the lens. Individuals with diabetes, pa-tients with history of retinal surgeries or those taking steroid medications are at higher risk of developing PSC.
Diabetic cataract
High levels of glucose in the lens can cause swelling and result in vi-sion changes. Ultimately, uncontrolled diabetes can perpetuate lens opacification and cause cataract formation.
Drug induced cataract
Although less common, cataracts can be induced by steroid medi-cations after ingested, inhaled or even local treatment.
Traumatic Cataract
These types of cataract can occur after blunt force or penetrating ocu-lar trauma.
Congenital or Polar Cataract
Although we often associate cataracts with older age, they can also be present at birth or can start developing shortly after. This type of cataract usual-ly grows adherent to the lens bag, which might cause higher risks for complications during surgery.
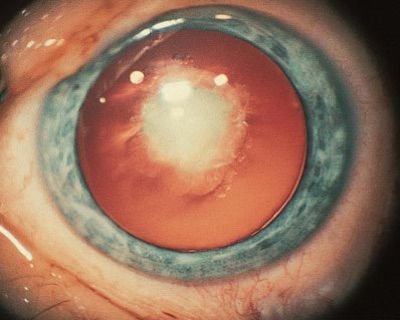
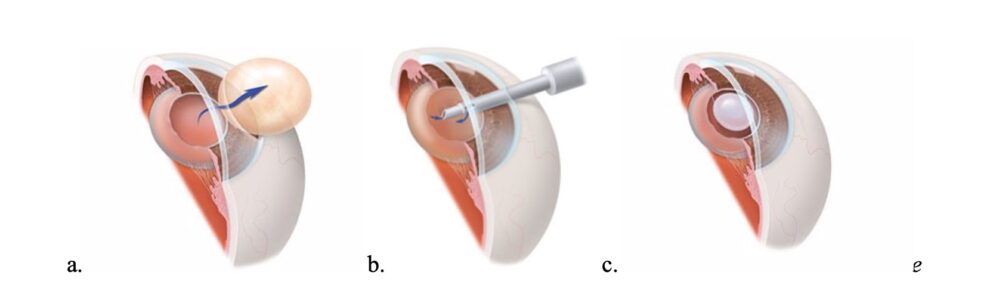
Cataract Surgery
Cataract surgery is one of the most common surgeries performed in our nation. Even though there are certain risk factors that can increase complications during surgery, the success and satisfaction rate is generally very high. Cataracts cause visual disturbances mainly because the clouding of the lens hinders adequate light from reaching the retina. During surgery, the cloudy lens is removed, and an artificial lens called an Intraocular Lens (IOL) is implanted inside the eye. Once the clear IOL is placed, light can focus on the retina without any impediment, resulting in clearer vision.
Images courtesy of aao.org
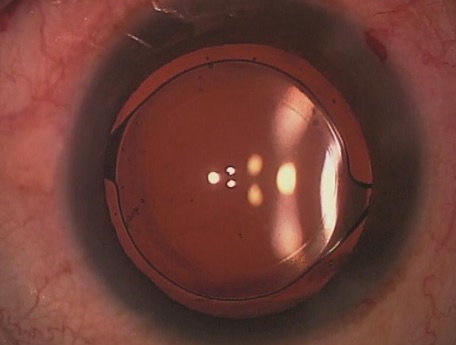
Image courtesy of aao.org
Advanced Options During Cataract Surgery
Use of Femtosecond laser
Dr. Josephson can either use manual methods or utilize femtosecond laser technology to break-down the opacified lens. During laser assisted excision, femtosecond laser replaces or assists the use of hand-held surgical tools for corneal incisions, anterior capsulotomy and cataract fragmenta-tion. It is important to note that Dr. Josephson can perform safe and successful surgery using man-ual methods. However, femtosecond laser will lessen the amount of energy used during surgery and can provide further independence from glasses by correcting mild to moderate astigmatism.
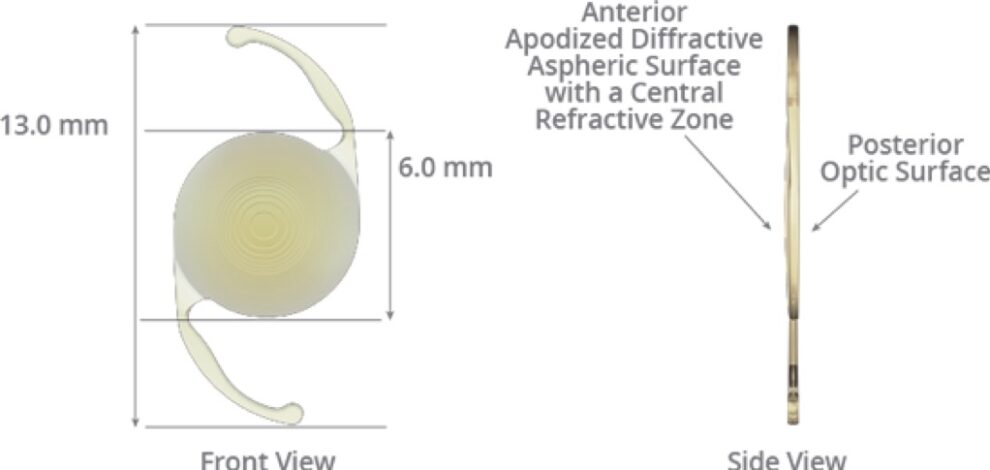
Image courtesy of myalcon.com
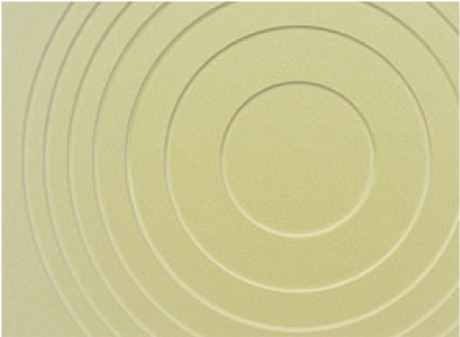
Image courtesy of myalcon.com
Different Types of Intraocular Lenses
Multifocal Lens
Multifocal intraocular lenses can expand the range of vision by providing a sin-gle elongated focal point. Therefore, by allowing an extension of visual range, this technology pro-vides more independence from glasses. It is important to note that these lenses are not accommoda-tive nor are they considered bifocal. Instead, they grant both distance and some near vision by uti-lizing diffractive optics. Some patients who use these lenses can see distance, intermediate and some near with limited glasses need. However, small print, needle work, low lighting, etc. will likely necessitate over the counter readers. Bear in mind that for patients with retinal diseases, these IOLs are usually not recommended since they could enhance certain visual disturbances.
Accommodative Lens
Accommodation is a process where the natural lens changes shape to fo-cus from near to distance and vice versa. In our forties, we start to lose this flexibility and become presbyopic, which forces us to rely on reading glasses to see objects up close. During cataract sur-gery, there is an option to select an IOL that simulates the natural lens. This intraocular lens is de-signed to flex and provide accommodation without using diffractive optics like the multifocal lens technology. It is our experience that there is variability in which patients gain more range in their vision. Small print will likely still require the aid of magnifiers.
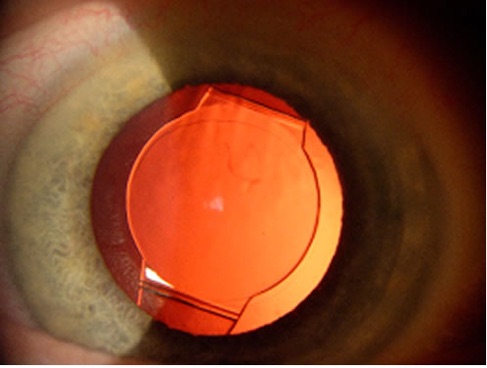
Image courtesy: Richard S. Hoffman, MD, I. Howard Fine, MD, and Mark Packer, MD, found on aao.org
Astigmatism Correction During Cataract Surgery
As discussed above, the femtosecond laser technology addresses mild to moderate astigmatism by making limbal relaxing incisions on the cornea. Comparable to the laser method, Dr. Josephson can also use handheld surgical tools to make these corneal incisions and correct astigmatism. For more moderate to severe astigmatism, toric lenses are utilized to give the most accurate and precise astigmatism correction at the focal point of the eye. There are monofocal, multifocal and accommo-dative toric IOL options that provide the sharpest vision for the desired focus without glasses or contacts.
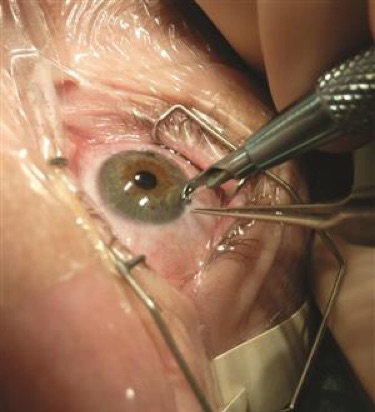
Image courtesy of aao.org
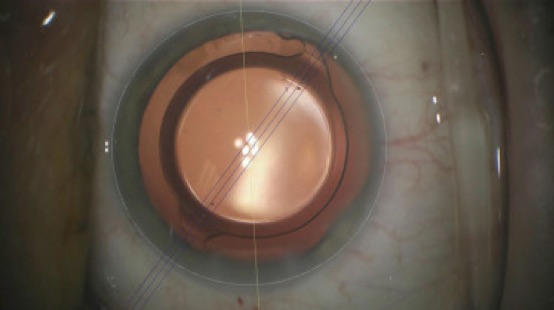
Image courtesy of aao.org
Intraoperative Lens Calculator
Occasionally, it can be difficult to obtain precise preoperative measurements if patients have a his-tory of refractive surgeries (LASIK, RK, AK etc…), mature cataracts or high eye prescriptions. In these cases, a technology called Intraoperative Lens Calculator (ORA) is available to measure the eye in the operating room and help determine the most accurate lens power. Moreover, this option can also be utilized if you have chosen to proceed with specialty lenses that provide range or cor-rect astigmatism.
Other conditions related to cataract surgery
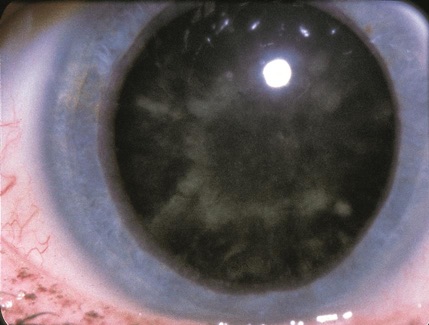
Pseudoexfoliation Syndrome (PXE)
This is an age-related systemic disease that manifests itself as tiny “dandruff like” flakes deposited on the front of the eye. This condition is also a risk factor for glaucoma because pseudoexfoliative material can obstruct the drainage system and lead to high eye pressure. Additionally, PXE can result in a challenging cataract surgery due to unstable lens structures. However, since it is usually diagnosed during a dilated fundus exam, Dr. Josephson and his team of surgeons will take extra precautions to ensure a safe and successful surgery.
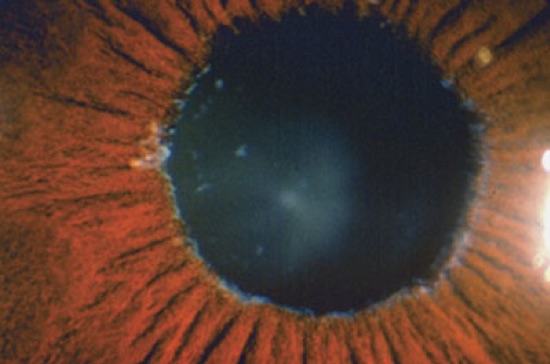
Image courtesy of aao.org
Posterior Capsular Opacification (PCO)
PCO is a postoperative physiological consequence of cataract surgery. During surgery, the surgeon removes the cloudy lens and places the artifi-cial lens inside our natural lens capsule. Through time, the back of the lens capsule can thicken or opacify. These changes can occur in a matter of months or years. This is NOT a recurring cataract, but it is rather caused by cell growth over the lens bag. When the capsule thickens, it hinders adequate light from reaching the back of the eye and ultimately results in blurry vision. This common condition can be observed without intervention if it is not visually significant. However, if vision is impaired, YAG laser capsulotomy can be considered. YAG capsulotomy is an in-office procedure where a laser is used to clean off the epithelial cells from the back of the lens capsule. Dr. Josephson will create a small hole in the center of the capsule, which al-lows more light to reach the retina. If you are experiencing blurry vision post cataract surgery, visit our office so that we can perform a dilated exam and direct you towards the right steps to achieve clearer vision.
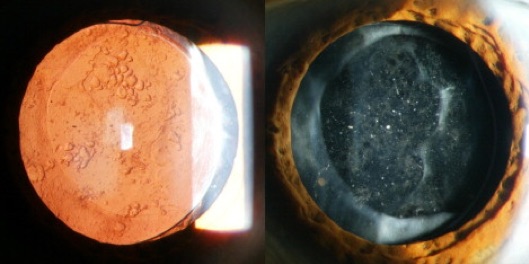
Image courtesy of aao.org
Glaucoma
Glaucoma is a group of diseases that damage the optic nerve, which is found in the back of the eyes and aids in transmitting messages to our brain. It can be easily detected through a comprehen-sive dilated exam and additional testing. During a glaucoma evaluation, you take a visual field test to assess your peripheral vision, your eye pressure is measured and so is the thickness of your cornea. Photographs of your optic nerves are also taken to gauge if any damage was inflicted by the disease. Damage from glaucoma is irreversible and there are no visual symptoms until it’s too late. Since a healthy optic nerve is necessary for good vision, damage can lead to peripheral vision loss or permanent blindness. Additionally, risk factors include pre-existing family history, age, ethnic background, high eye pressure, high blood pressure, and diabetes. Therefore, periodic test-ing is highly recommended to halt progression and commence treatment if needed.
Optic nerve
The optic nerve is responsible for our natural blind spot because it doesn’t contain any photoreceptors (rods and cons). However, the millions of nerve cells that make up the optic nerve transmit visual information from the retina to our brain. When assessing its health, eye care providers look at the cup to disc ratio of the optic nerve. The white “cup” or the central depression, does not send information to the brain and usually occupies less than half of the whole nerve. The optic disc on the other hand, is the healthy tissue surrounding the cup and aids in signal transmis-sion. Glaucoma causes cup enlargement by killing off the nerve fibers on the optic disc. This caus-es permanent peripheral vision loss and if uncontrolled, will result in blindness. Since this loss is irreversible, it is crucial to follow closely with an eye care provider as recommended.
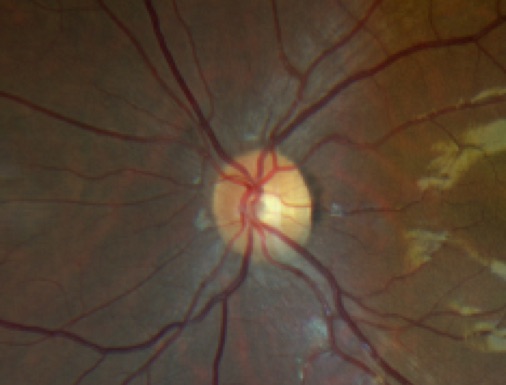
Image courtesy of Amen Nigussie
Glaucoma suspect
As we have similar arm lengths, our cup-to-disc ratio should also be similar sizes. Asymmetric cupping sizes of the optic nerves can be a concern for glaucoma. However, unequal cupping can be physiologic and might signify that the individual was born this way. If there are no signs of optic nerve damage, visual field defects or intraocular pressure elevation, the patient will be called a glaucoma suspect rather than being diagnosed with the condition. Biannual or yearly testing is highly recommended to detect changes and ensure glaucoma damage has not occurred on the nerve with the larger cup.
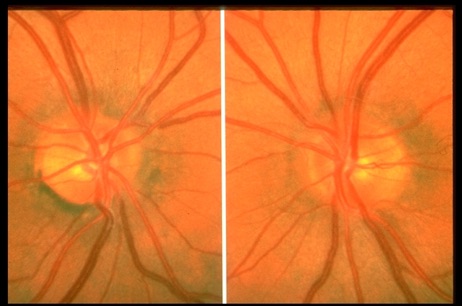
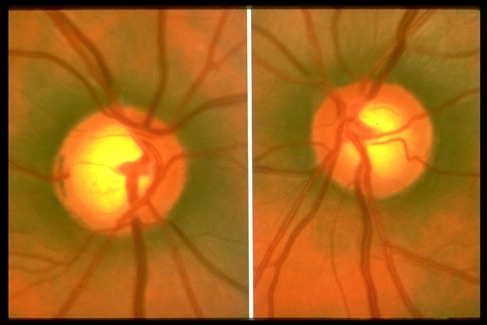
Image courtesy of aao.org
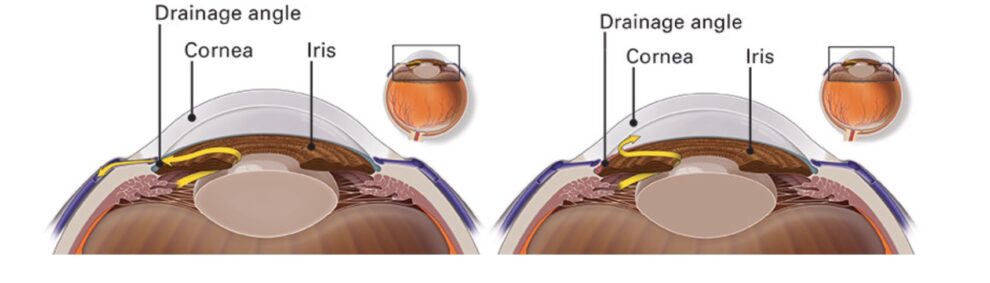
Open-Angle Glaucoma (OAG)
A clear fluid inside the eye, called the aqueous humor, continuously flows in and out of the anterior chamber. The fluid leaves the chamber through an open angle situated between the iris and cornea. Open-Angle Glaucoma (OAG) is caused by fluid buildup inside the eye, even though the drainage system or the angle, is open. This fluid buildup causes high eye pressure, which is damaging to the optic nerve.
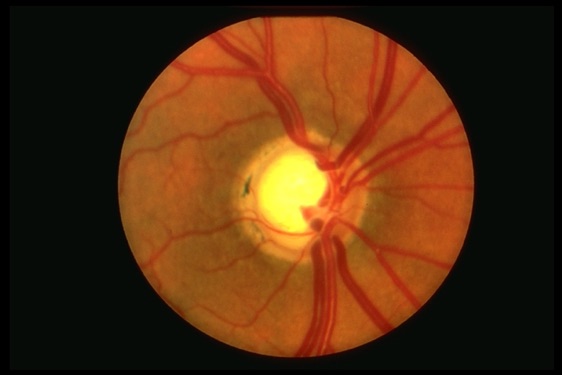
Image courtesy of aao.org
In Closed Angle Glaucoma (CAG), the structure of the eye makes it more likely that fluid drainage is obstructed or limited. Individuals who have narrow angles between the iris and the cornea are at a higher risk for this type of glaucoma. An acute episode of CAG is less subtle than the chronic form. The rapid rise in eye pressure can cause severe eye pain, nau-sea, eye redness, headaches, blurred vision, and halos. If you are experiencing these symp-toms, immediately call your ophthalmologist.
Lastly, damage to the eye channels, also known as the Trabecular Meshwork, can cause Traumatic Glaucoma. As mentioned above, if the drainage system is not working proper-ly, it results in elevated amounts of fluid inside the eye and ultimately raises the intraocular pressure. To ensure this system is not damaged, seeing an eye professional after a superfi-cial or penetrating eye injury is highly recommended.
Glaucoma Treatment
Glaucoma can be treated with eye drops, lasers, surgeries and stents. All these treatments are used to stabilize eye pressure, promote adequate fluid circu-lation within the eyes, halt further damage of the optic nerves and keep glaucoma under control.
- Drops: Glaucoma medication drops generally use two methods to stabilize intra-ocular pressure (IOP): by decreasing the production of the aqueous humor and/or through facilitating more liquid outflow. Since these drops utilize different method-ologies and have varying half-lives, it’s important to use them as instructed by the eye care provider to acquire the intended effects.
- Prostaglandin analogs: These increase aqueous humor flow by facilitating a mechanism of outflow that is different from the usual route. Example: lat-anoprost, Travatan Z, Xalatan, and Lumigan
- Cholinergic agonist: Encourage more aqueous humor outflow by utilizing the fluid’s normal route. Example: Pilocarpine
- Rho kinase inhibitors: Improve fluid drainage. Example: Rhopressa
- Beta blockers: Reduce aqueous humor production. Example: Timolol
- Carbonic anhydrase inhibitors: These decrease fluid production. Exam-ple: Azopt, dorzolamide (drops) or Diamox/Acetazolamide (pills)
- Alpha agonists: These drops use both suppression of aqueous humor pro-duction and increase outflow to reduce pressure. Example: Brimonidine
- Combination drops: Sometimes more than one drop is needed to attain ad-equate IOP reduction. During these instances, drops are either prescribed separately or as combinations. Some examples of combined medications are: Combigan, Cosopt, and Simbrinza
- Selective Laser Trabeculoplasty: SLT is a laser treatment that is used to lower eye pressure and subsequently decrease or even eliminate the use of glaucoma drops. During the procedure, the patient is placed in front of a machine and the ophthal-mologist will send several pulses of laser towards the trabecular meshwork, the structure in the eyes responsible for draining fluid. These laser shots induce in-flammation and cytokine release, which aid in cell to cell communication. By taking advantage of these biological processes, SLT increases trabecular cell proliferation, improve aqueous flow and ultimately decrease intraocular pressure. While it may take a few weeks to take effect, SLT results usually last 3-5 years and can be repeat-ed at any time if indicated.
- iStent: An iStent is a small apparatus implanted at the time of cataract surgery to help reduce intraocular pressure and decrease the number of glaucoma medications. This FDA approved procedure only adds a few minutes to cataract surgery but can have long lasting benefits for individuals managing glaucoma.
- Advanced surgeries: If drops and laser treatments are unable to control eye pres-sure, incisional surgeries like trabeculectomy and valve implants, are available to treat glaucoma.
Narrow Angles
A clear fluid inside the eye continuously flows in and out of the anterior chamber through an open angle situated between the iris and cornea. In individuals with an-atomically narrow angles, this drainage system can become compromised due to limited space and cause a dangerous spike in eye pressure. People with narrow angles should not be dilated because as the pupil widens, the space between the iris and the cornea further shrinks. This can put them at risk for developing acute angle closure glaucoma, which can present with high eye pressure, pain and even loss of vision. If you have anatomically nar-row angles, an ophthalmologist will likely recommend an outpatient laser therapy as a prophylactic treatment.
Treatment
Laser peripheral iridotomy (LPI) “opens” up a narrow angle by mak-ing a small opening on the iris, the colored part of the eye. This promotes normal fluid drainage and protects the eyes from permanent damage. The hole is not visual-ly significant and cannot be seen by the naked eye.