Eye Conditions
Overview
Dry Eye Syndrome
DES is caused by a chronic or sporadic lack of lubrication on the surface of the eye. For some individuals, dry eyes could be a result of either environmental or seasonal factors. However for others, systemic or physiological components can cause chronic ocular irritation, resulting in blurry vision, pain, and even decreased quality of life. Generally, dry eyes can be caused by excessive computer use (don’t forget to blink!), contact lens wear, medications, or lagophthalmos – the inability to fully close one’s eyelids. In addition, diseases such as diabetes, thyroid disorders, rosacea, lupus, rheumatoid arthritis, and Sjogren’s syndrome, will affect tear film production. Management for dry eyes include: artificial tears and gels, medication drops, serum tears, punctal plugs, stem cell therapy, and IPL laser treatments. Furthermore, treating underlying conditions like blepharitis or lid malpositioning, can alleviate these symptoms.
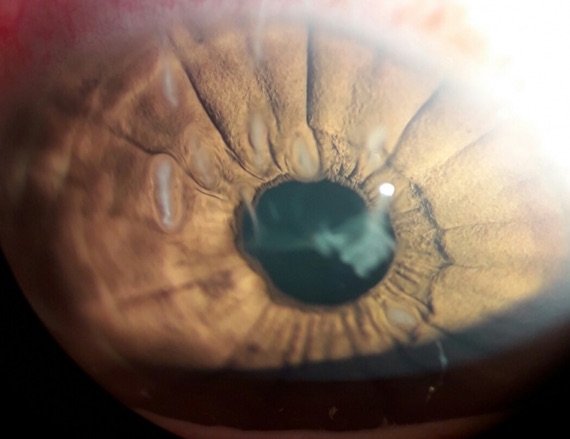
Image courtesy of aao.org
Blepharitis
Blepharitis is a chronic inflammation of the eyelids and commonly occurs when the oil glands located on the eyelids are blocked. This causes the lids to become irritated and even appear greasy. Individuals with blepharitis usually wake up with crusty eyelashes or with lids that are stuck together. Additionally, the surface of the eye can be affected due to abnormal oily secretions and debris from lashes. This irritation can lead to dryness, blurry vision, foreign body sensation, and excessive tearing. Certain organisms such as Demodex might also exacerbate the inflammation around the eyes. Therefore, it is essential to practice consistent lid hygiene and incorporate warm compresses and lid wipes into one’s daily regimen. Since ocular rosacea may also be another factor for chronic inflammation, physicians might prescribe oral antibiotics (doxycycline) to promote healthy oil secretion and ultimately minimize inflammation.

Image courtesy of aao.org
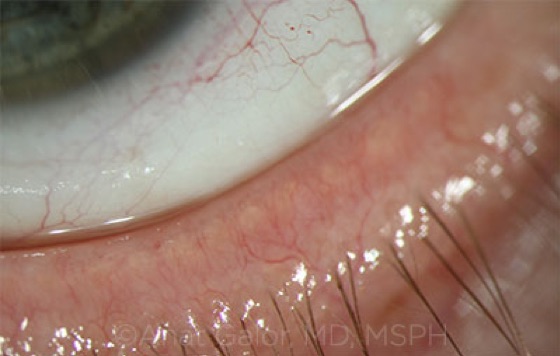
Image courtesy of aao.org
Chalazion
Chalazia are benign bumps that arise on the upper or lower lids and are caused by clogged oil glands. These cyst-like nodules usually drain on their own. However, frequent use of warm compresses, gently massaging the surface, lid wipes, and topical steroid ointments can speed up the process. If these treatments are unsuccessful, an ophthalmologist can perform an incision and drainage to remove them. Although a chalazion is not visually threatening, if it grows big enough it can press on the cornea, and could cause mildly distorted vision. Additionally, the frequency and amount of chalazia growth can be exacerbated by conditions like blepharitis or ocular rosacea due to chronic eyelid inflammation. If you have these conditions, you can prophylactically use lid wipes, oral antibiotics and warm com-presses to halt further eyelid irritation.

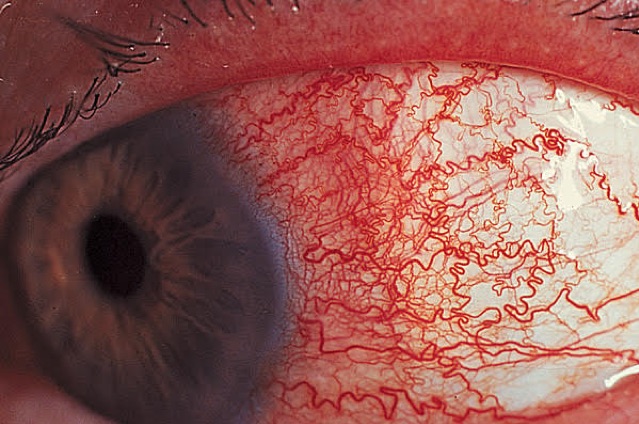
Pterygium
This is a pink or fleshy non-cancerous growth that starts from the white surface of the eye and can slowly extend to the cornea. Pterygiums are usually caused by significant exposure to ultraviolet light. Therefore, it’s most common in individuals who live near the equator. Other irritants like dust and wind can also aggravate symptoms. Therefore, it is very important to wear sunglasses with UV protection and use artificial tears frequently to minimize irritation. Pterygiums can cause constant foreign body sensation, eye redness, dryness and irritation. Additionally, if they grow on the cornea, they can change the shape and become visually distorting. In this case, Dr. Josephson or Dr. Ong will likely recommend a surgical intervention or will closely monitor for any increase in size.

Image courtesy of aao.org
Pinguecula
Pinguecula is a noncancerous yellowish bump presenting on the white part of the eye. This is usually caused by sun damage and wind exposure. Pingueculas can cause dryness, foreign body sensation, redness and irritation. Symptoms can sometimes be alleviated by frequent use of artificial tears and using sunglasses with UV light protection to avoid further damage. Since reoccurrence is possible after removal, patients should closely consider the risks, benefits and alternatives before pursuing a surgical intervention.

Iritis
Iritis is the inflammation of the colored part of the eye, also known as the iris. Symptoms include: redness, pain, light sensitivity, and sometimes decreased vision. This can be caused by injuries, infections, genetic factors, or due to an autoimmune response. This is usually treated with topical steroid drops to help reduce the inflammation. Dilation drops can also aid in diminishing pain by freezing the pupil in position and minimizing iris spasm. If this is reoccurring, your eye care provider will likely order an autoimmune workup since iritis can be an indication for underlying autoimmune conditions.

Uveitis
Uveitis is an inflammation of the middle layer of the eye, known as the uvea. However, this disease can also extend to other parts such as the lens, the optic nerve as well as the retina. Since there are different types of uveitis, which are mainly classified by the area of inflammation, an ophthalmologist will construct a treatment plan based on the symptoms the patient displays. Symptoms can include: pain, light sensitivity, eye redness, floaters, increased eye pressure, and blurry vision. Although the cause might sometimes be ambiguous, uveitis can manifest due to systemic, inflammatory, or autoimmune conditions. This disease can also be induced by eye infections or trauma. Finally, since uveitis can lead to permanent complications if left untreated, it’s crucial to be closely monitored by an eye care provider.
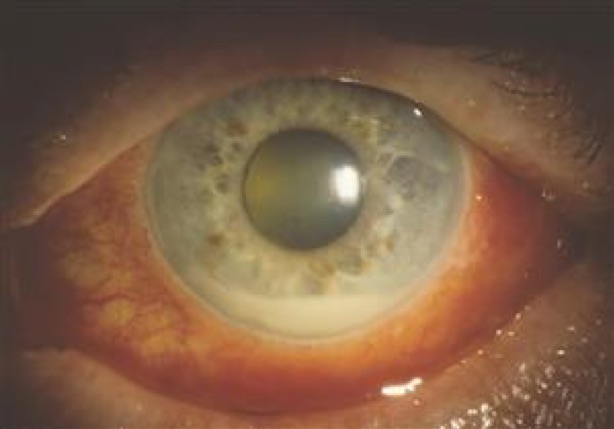
Image courtesy of aao.org
Scleritis
Scleritis is a condition when the white part of the eye, also known as the sclera, becomes inflamed. Although this could be caused by infection or trauma to the eyes, autoimmune disorders are usually found to be the underlying issue. Individuals with rheumatoid arthritis, lupus, Sjögren’s syndrome, etc. can experience recurrent episodes of scleritis. Symptoms include an inflamed or red sclera, deep aching pain that extends to the face, blurry vision, and photophobia. Usually, NSAIDs like ibuprofen are recommended due to their pain relieving as well as anti-inflammatory properties. Your ophthalmologist might also order blood tests to rule out any autoimmune disorders. If indicated, it is important to establish care with a rheumatologist and receive systemic treatment with oral steroids and biologic drugs.