Cornea
Overview
Anterior Basement Membrane Dystrophy
ABMD; also known as Map-Dot-Fingerprint Corneal Dystrophy is an inherited disorder of the cornea. It may present as re-current corneal erosions and blurry vision. Your eye care provider will likely advise ag-gressive lubrication and the use of overnight NaCl ointments. If symptoms persist, superfi-cial keratectomy and an amniotic membrane transplant will be recommended. This proce-dure consists of removing superficial cells to obtain a clear corneal bed. Afterwards, a stem cell membrane is placed to help revitalize and clear up the surface.
Band-Shaped Keratopathy
BK is a line or band that appears on the cornea. This is formed due to calcium precipitates that are deposited on the surface of the eye. If advanced, it can cause blurry vision, irritation or redness. Techniques like manual superficial keratec-tomy, phototherapeutic keratectomy or a chelating agent like EDTA, are utilized to treat this condition.
Corneal Abrasion
An abrasion is caused by disruption or cell loss in the corneal epitheli-um, the top layer of the cornea. A scratched corneal surface can result in discomfort, pain, redness and photophobia. To treat this condition, your doctor might recommend antibiotics, pressure patching, aggressive lubrication or a bandage contact lens for pain relief and speedy healing.
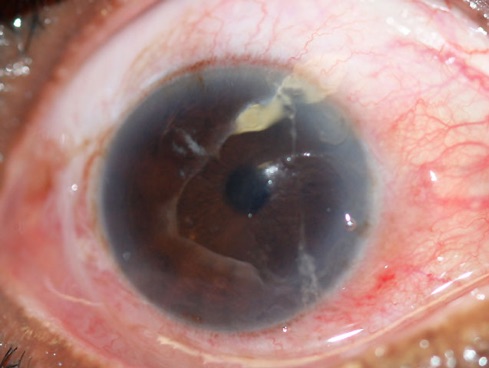
Corneal Ulcers
Although corneal ulcers are typically bacterial in nature, they can also oc-cur from fungal, parasitic or viral infections. Contact lens wearers are especially susceptible for corneal ulcers because the material rubs against the surface of the eye enabling infection. Therefore, it is necessary to practice good hygiene to decrease the risk of ulcers. If left un-treated, corneal ulcers can cause permanent damage or even blindness. Symptoms include eye redness, pain, excessive tearing, foreign body sensation or blurry vision. Corneal ulcers are usually treated using antibiotic drops and these medications will be used frequently until infection subsides. Your doctor might also recommend sending a culture to pathology to determine the best course of treatment.

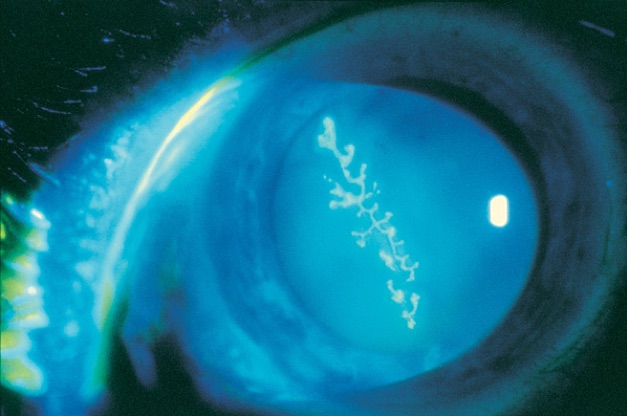
Ocular Herpes
Herpetic eye diseases are usually caused by herpes simplex 1, the virus that causes cold sores or varicella-zoster, the culprit for chicken pox and shingles. Ocular herpes can produce sores on the surface of the eye, leading to redness, blurry vision, pho-tophobia, pain and foreign body sensation. In addition to these symptoms, herpes zoster can present with lesions on forehead or around the eyes. To treat ocular herpes, oral antivi-ral medications are prescribed to reduce the risk of inflammation and permanent scarring on the cornea. Antibiotic drops are indicated to prevent a secondary bacterial infection and once the infection subsides, steroid drops are prescribed to lessen inflammation. Finally, since viral eye infections can be recurrent, your doctor might suggest a maintenance dose of antiviral pills to suppress any outbreaks.
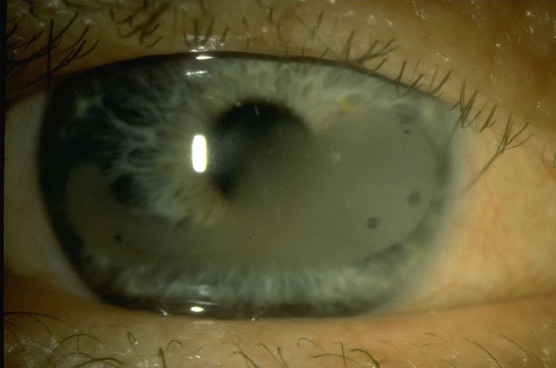
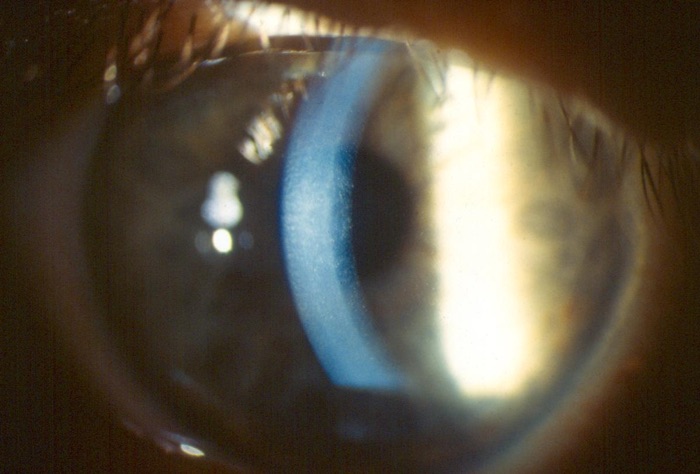
Fuchs’ Corneal Dystrophy
Fuchs’ dystrophy occurs when the endothelium layer of the cornea, which is responsible for pumping out excess fluid, undergoes degenerative chang-es. As these cells die off, the cornea becomes edematous, leading to a swollen and puffy surface. This bilateral condition usually affects people after age 50 and symptoms include: glare, cloudy vision and eye discomfort. During early stages, hypertonic NaCl ointment is used to remove excess fluid out of the endothelium through osmosis. If the swelling does not come down with topical treatment, it can lead to painful blisters called corneal bullae. If symptoms do not subside, a surgical intervention will be considered. Dr. Josephson and his team of surgeons will recommend a partial thickness corneal transplant (DSAEK or DMEK) to replace the endothelium.
Keratitis
Keratitis is an inflammation of the cornea, which can result from injuries, auto-immune diseases, contaminated contact lenses, eye lid disorders or infections (Corneal Ul-cers). Symptoms include redness, pain, excessive tearing, photophobia or foreign body sensation.
Keratoconus
This is a condition where the dome shaped cornea begins to bulge outward like a cone. Normally, proteins called collagen fibers help the cornea maintain its natural shape and prevent it from steepening. However, if these collagen fibers begin to weaken, the cornea changes into a football shape and progressively thins. Keratoconus can be de-tected as early as adolescence and risk factors include genetic predisposition, excessive eye rubbing and chronic eye irritation. This condition is visually significant because a thinning cornea can result in light rays going out of focus, which ultimately causes blurry, fluctuat-ing and distorted vision. Due to the cornea’s irregular shape, patients are often unable to gain optimal vision by using glasses or soft contact lenses. Therefore, individuals with ker-atoconus usually wear specialty contacts like scleral lenses or rigid gas permeables. If the cornea progressively thins and further changes its structure, vision correcting contact lenses can be uncomfortable to wear for extended periods of time. To halt progression and to help strengthen the collagen fiber bonds, a procedure called collagen cross linking is recom-mended. However, in cases where the cornea becomes dangerously thin or severe scarring is noted, a corneal transplant might be the only possible course of treatment.

Interventions for Keratoconus
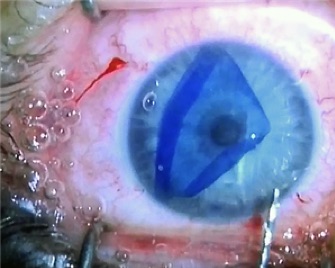
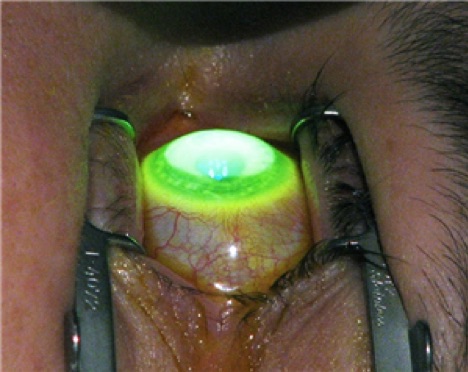
Epithelium-off Collagen Cross Linking
As mentioned above, collagen cross linking strength-ens the corneal tissue and stops it from further thinning and bulging out. During this FDA ap-proved outpatient procedure, an ophthalmologist first removes the surface eye cells called the epi-thelium. Afterwards, liquid riboflavin (vitamin B2) is periodically placed on the eye after exposure to a controlled amount of ultraviolet light. This stabilizes the cornea by creating new links between the collagen fibers. Cross linking can significantly reduce the need for a corneal transplant and can even make contact lens wear more bearable.
Intacs
Intacs are plastic inserts that are placed in the eye to reshape and flatten the steep portion of the cornea. This vision correcting procedure helps eliminate or lessen astigmatism in keratoconus patients, so they can obtain functional vision.
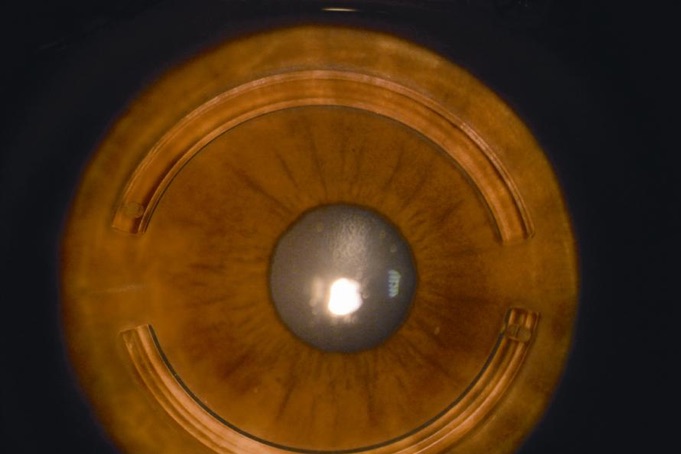
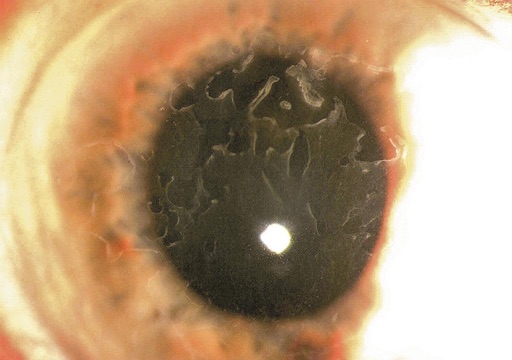
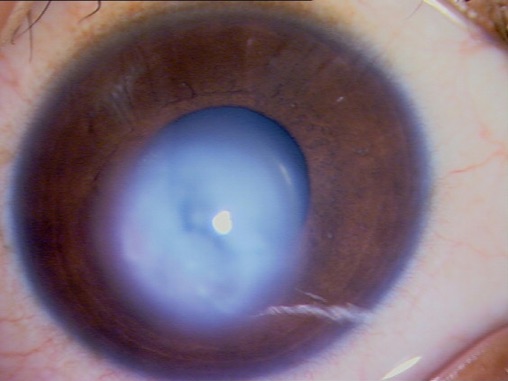
Corneal Hydrops
In certain advanced keratoconus cases, the cornea becomes edematous (swells up with fluid) and takes on a milky-white appearance. This acute episode results in extreme light sensitivity, blurred vision, pain and permanent corneal scarring.
Corneal Transplants
Corneal transplants are used to treat irreversible damage inflicted by corneal conditions like: kerato-conus, Fuchs’ dystrophy, ulcers, trauma and scarring. Corneal transplants are done routinely and have a relatively high success rate. Donor tissues are obtained from eye banks and are readily available when needed. Additionally, corneal tissue typing is not essential since there are no blood vessels spanning a healthy cornea. Therefore, this significantly decreases an immunological re-sponse and the risk of rejection. Listed below are the different types of corneal transplants.
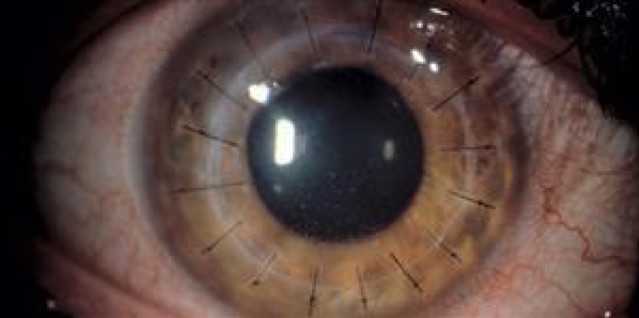
Penetrating Keratoplasty (PKP)
This procedure, also known as full thickness corneal transplant, utilizes a technique that has been around for many years. Unlike partial thickness techniques, the surgeon performs a full thickness resection of the cornea and replaces it with a donor tissue. Afterwards, the tissue is held in place with continuous or interrupted sutures, which will be removed sequentially post-surgery. In PKP, postoperative recovery time can take relatively long and will likely delay the best-corrected visual potential. Cur-rently, for conditions such as Fuchs’ dystrophy that do not need a full thickness resection, PKP has been replaced by newer procedures that utilize a tissue-for-tissue approach. How-ever, this older technique is still used for keratoconus, severe corneal scarring or for cases that span multiple layers of the cornea.
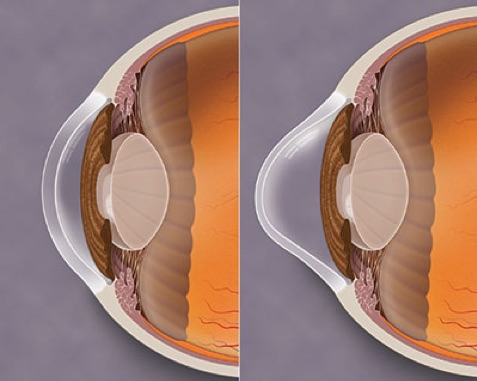
DSEAK
Unlike PKP, this method only replaces the damaged cell layer instead of the full thickness of the cornea. This procedure is used to treat endothelial conditions such as Fuchs’ dystrophy. During surgery, the endothelium and Descemet membrane are removed and replaced with donor endothelium and stroma tissue that is 100-200 microns thick. Af-terwards, an air bubble is inserted with a syringe to enforce adherence to the rest of the re-cipient’s cornea. Post-surgery, the patient will be required to lay down flat, eyes towards the ceiling, for a few days until the air bubble is completely gone.
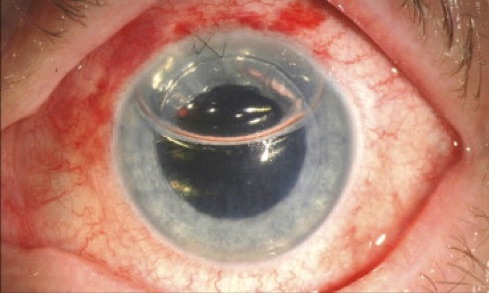
DMEK
This newer method literally replaces tissue for tissue. Unlike DSEAK, the donor tissue doesn’t include corneal stroma but only contains the Decement membrane and endo-thelial layers. This makes the graft approximately 10-15 microns thick. After transplanta-tion, an air bubble is placed to help the tissue stick and the patient will continue lying down flat until bubble dissipates. Since less tissue is transplanted, it may result in better visual po-tential and quicker recovery. However, the DMEK procedure has a higher chance of requir-ing multiple post-surgical office visits. If tissue is not fully adherent, Dr. Josephson may want to add more air to help facilitate full adherence. Typically, if a patient has transporta-tion issues or concerned about lying supine for additional days, it may be advisable to pro-ceed with the DSEAK procedure.